(Mercola) If you’ve been trying to lose weight and making serious diet cuts in all the right places for weight loss, not just maintenance, but still not making progress, there may be something at play that is effectively blocking your success. According to new research, the problem might not be what’s already there, but what’s missing — specifically the right gut microbiota. Research at the University of Copenhagen, Denmark, found that the ratio between two types of gut microbes, Prevotella and Bacteroides, evidenced this premise.
For 26 weeks, 62 individuals with increased waist circumference were randomly assigned to either the typical diet enjoyed by the average Dane, or a low-fat, high-fiber diet that included fruits, vegetables and grains. At the end of the study,1 feces samples revealed that the people on the high-fiber diet with a high Prevotella-to-Bacteroides ratio (P/B ratio) lost an average of 10.9 pounds of body fat, which was 3.5 more pounds than the others.
As The New York Times noted,2 those on the regular diet with a high Prevotella ratio lost 4 pounds, compared with 5.5 pounds for those with a low Prevotella ratio, which was statistically insignificant. In short, the researchers concluded, “subjects with high P/B–ratio appeared more susceptible to lose body fat on diets high in fiber … than subjects with a low P/B-ratio.”3
The key in weight loss success, as well as the difference, according to lead author, Mads F. Hjorth, an assistant professor at the University of Copenhagen, is that losing fat, rather than muscle mass, is what delivers a meaningful bottom line. Hjorth admitted that while studying the microbiome — the ecosystem of microorganisms in your gut — has, as yet, brought little in the way of practical results, their newest findings may end up being something they can use as a practical tool to aid in weight loss and overall health.
Beyond Weight Loss: Probiotics to Help Prevent and Treat Colon Cancer
Scientists in the U.K. took a hard look at how the introduction of probiotics might change gut microbiomes and found it not only may help prevent the formation of tumors but even treat existing ones.4 In fact, their research,5 published in The American Journal of Pathology, found that the gut bacteria Lactobacillus reuteri has the potential for treating colon cancer, the third most common cancer in the U.S. other than skin cancer.
Several studies, including one in Malaysia6 and at least one intensive review7 of many studies targeting the subject, had already determined there are several factors that increase incidence of colorectal cancer, such as having been diagnosed with inflammatory bowel disease, certain genetic factors, lack of exercise, red meat intake, low vegetable and fruit consumption, whether or not you smoke, and being overweight or obese.
The upshot of The American Journal of Pathology study, led by Dr. James Versalovic, a professor of pathology and immunology at Baylor College of Medicine in Houston, is that your gut microbiome is a huge player in your overall health, including playing a role in the development of colorectal cancer.
While many of the mechanisms involved weren’t immediately known, research indicates probiotics can play a starring role in its prevention, with Lactobacillus reuteri, a naturally occurring probiotic in mammals, observed as reducing intestinal inflammation.
For the study, researchers administered L. reuteri to HDC-deficient mice (as well as using other mice given a placebo for comparison) to regulate their immune responses for observation. DSS, a substance that stimulates inflammation, was used along with azoxymethane, a carcinogenic chemical, to induce tumor formation. The actual mice studies took place 15 weeks later.
Study Procedures and Proof Positive for Probiotics
Using positron emission tomography to scan for tumors, scientists observed that the probiotic-treated mice had fewer tumors, and the ones they had were smaller in comparison with the placebo mice, whose tumors were larger and greater in number.
Medical News Today explained:
“In adult mice, it has been noted that the lack of an enzyme called histidine decarboxylase (HDC) made the animals significantly more susceptible to developing colorectal cancer associated with inflammation of the bowels. HDC is produced by L. reuteri and helps to convert L-histidine, which is an amino acid with a role in protein synthesis, to histamine, which is an organic compound involved in the regulation of the immune response.”8
Two more items were deemed significant in the studies: inactive, HDC-deficient strains of L. reuteri exhibit zero protective effects, and the active strain of the probiotic even decreased inflammation caused by the DSS and azoxymethane chemicals given to the mice. Versalovic summed up the trials:
“Our results suggest a significant role for histamine in the suppression of chronic intestinal inflammation and colorectal tumorigenesis (tumor formation]). We have also shown that cells, both microbial and mammalian, can share metabolites or chemical compounds that together promote human health and prevent disease.”9
In this study, too, scientists are said to be unsure about the function of histamine in humans in relation to cancer, which is interesting since among 2,113 people with colorectal cancer, data “suggested” that those with higher levels of HDC have a better survival rate. The team asserted that probiotics help convert L-histidine into histamine, which could be used to both lower colorectal cancer rates and aid treatment, and Versalovic concluded:
“We are on the cusp of harnessing advances in microbiome science to facilitate diagnosis and treatment of human disease. By simply introducing microbes that provide missing life substances, we can reduce the risk of cancer and supplement diet-based cancer prevention strategies.”10
‘Borrow’ Younger Gut Microbes to Increase Longevity
Studies on fish introduced the novel idea that gut microbes injected into older individuals might also inject more vim and vigor, while also helping them live longer. Some of the world’s shortest-lived vertebrates, turquoise killifish that swim in short-lived ponds formed by rainy seasons in Zimbabwe and Mozambique, were the lucky recipients of gut microbes from slightly younger fish — lucky because they lived longer.
A research team from the Max Planck Institute for Biology of Ageing in Cologne, Germany, arranged for older killifish — middle-aged at 9.5 weeks — to ingest the gut microbes belonging to killifish only 6 weeks old. Nature reported:
“The transplanted microbes successfully recolonized the guts of the fish that ate them, and extended their lives. The median life span for these animals was 41% longer than that of fish exposed to microbes from middle-aged animals, and 37% longer than for fish that received no treatment.
At 16 weeks — old for killifish — the individuals that received gut microbes from young fish were more active than other elderly fish, with activity levels more like those of 6-week-old fish.”11
Bulletproof 360 equated the concept with cutting-edge science that wages war on aging using an “experimental technique” called parabiosis,12 an allegedly 150-year-old science that connects the vascular systems of old and young animals to see how the exchange of blood might impact their health, behavior and anything else that might change.
But rather than using blood, scientists used the contents of the guts — poop — in the killifish microbe exchange, aka fecal transplantation therapy, as they, just like humans, are full of a comparable set of good and not-so-good gut bacteria. It’s difficult to say how the fish were feeling, but they appeared to be livelier and more active upon receiving the younger microbes.
The Importance of Good and Bad Gut Bacteria
When your gut microbiome is balanced, your general function, like the fish, is one that reflects a boost in energy because all-around, you’re healthier. When your microbiome is lacking in healthy bacteria, as researchers report, you feel physically depleted and your performance suffers.
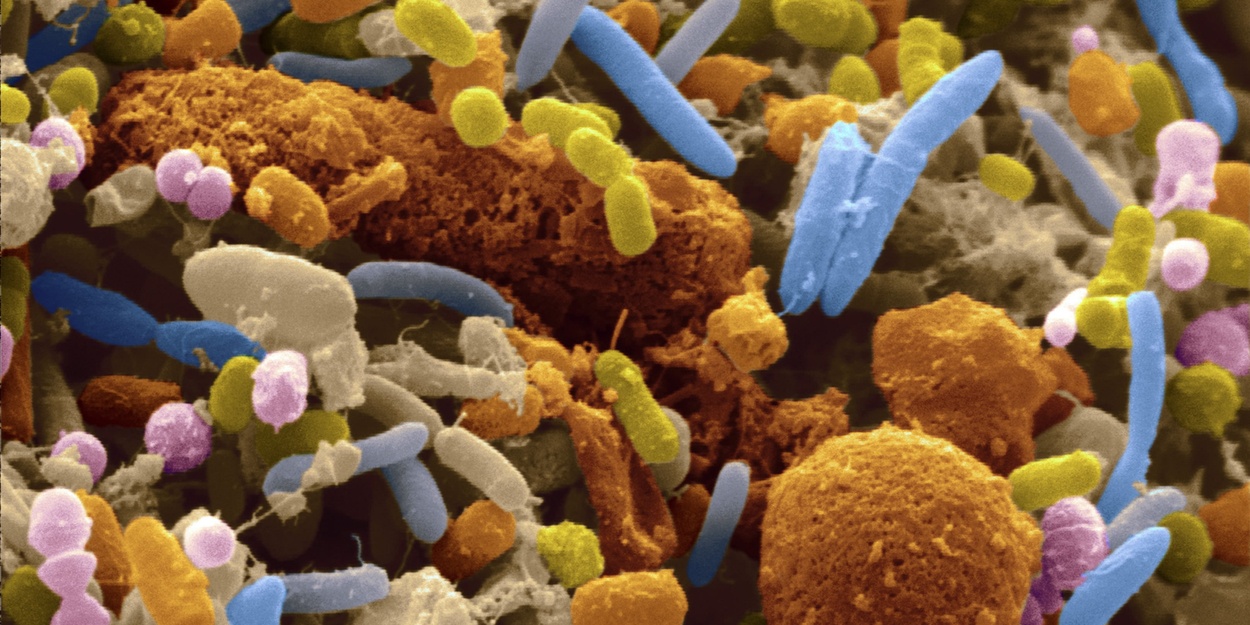
Not surprisingly, your microbiome profile can change as you age. Your body consists of around 100 trillion microbes that, when properly balanced, protect your gut, your immune system function and, consequently, your overall health. Here’s how it works:
“Gut microorganisms help you digest your food, and byproduct from the microbes eating your food (yes, it’s bizarre but it works) can be helpful to your system. Around 75 percent of your vitamin K supply is produced in the intestines by gut bacteria. Gut bacteria also help your body make its own B vitamins and absorb the B vitamins that come from food.”13
Many factors can change your gut health, for better or worse, including those listed in the table below:14
You’ll notice there’s one more factor that can affect the balance of your gut bacteria, and that’s age. You may also notice that other than age, all the rest of the above can be controlled. If you’ve ever marveled at the way a 5-year-old can tear up a playground for hours, and college students can stay up studying night after night without seeming to be adversely affected, gut microbiomes, to a large degree, can be thanked.
The fact is, the gut health of older individuals tends to be vastly different from those of people much younger, and it changes energy levels, cognitive function, muscle strength and immunity, studies say.15 The good news is that healthy gut bacteria can make all the difference in the way you age.16 Taking good care of yourself by paying attention to the items on the above table is not just wise for protecting your health now, but for your future health and even your chances of living longer.
Getting Your Own ‘New’ Gut
Your health is often a direct result of behaviors you engaged in last week, last year and even decades ago, depending on your age. Scientists have linked diseases like Parkinson’s and chronic fatigue to the microscopic organisms and bacteria in your gastrointestinal tract.17,18 Taking prescription medications is another way your body can be thrown out of whack, including combinations of drugs you might be taking that often cause serious and even deadly side effects and health issues.
In fact, it’s not your genes that determine your longevity, as some believe, as in “My grandfather and my father both died of heart disease, so I probably will, too.” Research strongly supports environmental factors as being responsible for the diseases that plague so many people.
It’s the expression of your genes that counts, and that is heavily influenced by your lifestyle choices. Even up to 90 percent of a person’s cancer risk is due to changeable factors such as the items listed above, while only 10 percent can be attributed to genetic defects, one study affirms.19
Nourishing your gut bacteria is one of the most crucial steps in maintaining health, and that can be done by eating traditionally fermented foods such as raw grass fed yogurt, kefir and fermented vegetables, which you can make at home, and foods containing fiber, such as nuts and seeds, fruits and vegetables, and other foods to promote better digestive health.
Probiotic supplements can also be beneficial. Avoiding sugar, as well as processed, packaged foods, will go a long way toward balancing and optimizing your gut health. The more you take care to develop gut health. The more it will help increase your energy, improve your sleep, balance your stress levels, diminish your risk for cancer and other diseases and even help you lose weight. Making small changes now will pay big dividends in the way you think, feel and function.