This is an excerpt from the extensive article Best Supplements To Kill Lyme and Everything Else You Ever Wanted To Know About Lyme Disease.
Current diagnostics miss up to 60% of acute cases. This is what’s so infuriating for those trying to figure out what’s going on with their bodies: Testing for Lyme is inaccurate, but especially so in the beginning. By the time the tests are likely to show positive for someone with Lyme, antibiotic treatments are typically no longer effective. In other words, people would go to their doctor and ask if they have Lyme, the doctors would say how rare it is (fortunately doctors are getting much better about this lately), but would reluctantly perform the tests, only to find no trace of Lyme. So the person would assume some other autoimmune disease while the Lyme slowly proliferates. Then the person would eventually seek another opinion, get another round of tests, and maybe (but often not) find out they do in fact have Lyme. Or, they often find out that one can have Lyme and still test negative indefinitely, but at this stage, the person is showing enough symptoms that the new more knowledgeable doctor can easily conclude that it’s Lyme.
But now the antibiotics will no longer be effective. It’s too late. Many people try anyways, wrecking their immune system in the process.
I suspect that often times a heavy round of antibiotics works to kill the bacteria, but the body is left so badly damaged that new infection (often Candida being the first) takes over, and all of the symptoms remain.
Borrelia does not seem to circulate in the blood. This is the main reason it is so difficult to detect. The bacteria also have a very slow replication rate, so the number of bacteria found in a host remains small, at least for a long time.
There are multiple tests for Lyme. The CDC recommends screening with the ELISA test and then confirming the results with the Western blot test. As mentioned, these tests are completely unreliable during the first 4-6 weeks of infection. The tests only measure the patient’s antibody response to the infection, not the presence of the bacteria itself.
Lyme disease is notoriously difficult to diagnose using conventional tests. And there’s great variation in the presentation of the disease as well, depending on where you contracted it, and whether or not you have any other coexisting infections. There is a group of seven or eight microbes that are the most common. The worst ones are Babesia microti and the different forms of Bartonella.
It is said that an initial course of antibiotics given in stage one cures the disease most of the time, but why not all the time? Is the course of antibiotics too short? Should more be given? Should they be given long term, especially for those who have stage 3 symptoms? What if blood tests no longer show spirochetes? If the antibiotics don’t work, the patient now has to combat Lyme with a very depleted immune system.” – Dr. Dietrich Klinghardt, MD, PhD
Why Antibiotics May Not Work for Lyme Disease
These days, early treatment is typically successful, according to the latest science, but most patients go undiagnosed for years. At least 20% of those who are said to be successfully treated for Lyme will experience the same symptoms after treatment, which as mentioned, can easily be attributed to a depleted immune system leading to Candida overgrowth or other fungal pathogens, opening the door for many other infections as well.
Antibiotic resistance occurs at a high rate with spirochete bacteria. Borrelia (and also its co-infections), will respond slowly to antibiotics. They will develop resistance. The bacteria that survive antibiotics can become completely antibiotic resistant. This is why doctors are starting to use multiple antibiotics at once seems, and this does lead to better chance of defeating Lyme, and depleting the immune system. If the medication fails, the bacteria that have survived will not only become resistant, but it will also become much more entrenched in the host.
The Lyme Timeline
Phase One – 3 to 30 Days
Also called early localized infection
Some say less than 50%, others say up to 70-75% develop the bullseye rash, starting at the site of the tick bite. It is not itchy or painful but they are usually warm to the touch. Sometimes flu-like symptoms develop soon after, including fever, chills, swollen lymph glands, headaches, muscle pain, and joint pain.
Phase Two – Days to Weeks After Bite
Also called early disseminated infection
- Rash spreads
- Large joints may become swollen and painful
- Stiff neck in some cases
- Meningitis may develop
- Dizziness
- Heart palpitations
Phase Three – Later Months to Years
Also called late disseminated infection
Many infectious disease specialists believe that “chronic Lyme disease” does not exist, and that Lyme disease from a tick bite can be cured with a short course of antibiotics. It is possible that those who have undergone antibiotic treatments are suffering from the side effects of antibiotics, but more and more experts are coming around to the idea that Lyme disease can survive and cause long-term autoimmune symptoms when antibiotics don’t work. We all know (or at least, we all should know) that antibiotics do not always work and can cause more problems.
- Arthritis symptoms – swollen, painful joints (fluid-filled joints)
- Neurological symptoms – numbness, tingling, shooting pains
- Cognitive symptoms – brain fog, short-term memory deficits, confusion
- Mood disturbance – depression
- Fatigue
- Abnormal heart rhythms and heart failure
Facial paralysis sometimes occurs in this stage or stage two.
Scary Lyme Facts You Should Know
How does Lyme make us sick, and why is it so damn resilient?!?!
- Spiders, mosquitoes, fleas, and mites may also be spreading the same or similar bacterial infections.
- Tests are unreliable because they measure the patient’s antibody response to the infection, not the bacteria itself.
- There’s great variation in the presentation of the disease, depending on where it’s contracted, and whether there are other coexisting infections. At least eight other microbes make up the most common co-infections., including Babesia microti and different forms of Bartonella.
- Borrelia burgdorferi, the bacteria that causes Lyme disease, has a corkscrew shape that allows it to bore deep into tissues and cartilage (including the brain and nervous system), safely out of reach of most antibiotics.
- Borrelia burgdorferi can give up its corkscrew shape and convert to a form that is able to live inside cells (“intracellular”) where again, antibiotics have less reach.
- Borrelia burgdorferi, along with other similar microbes, can form dormant cysts that are completely resistant to antibiotics; the harder you hit it, the more resistant it becomes.
- Most ticks carry multiple disease-causing pathogens called co-infections. Borrelia burgdorferi is usually accompanied and aided by co-infections of other stealth microbes.
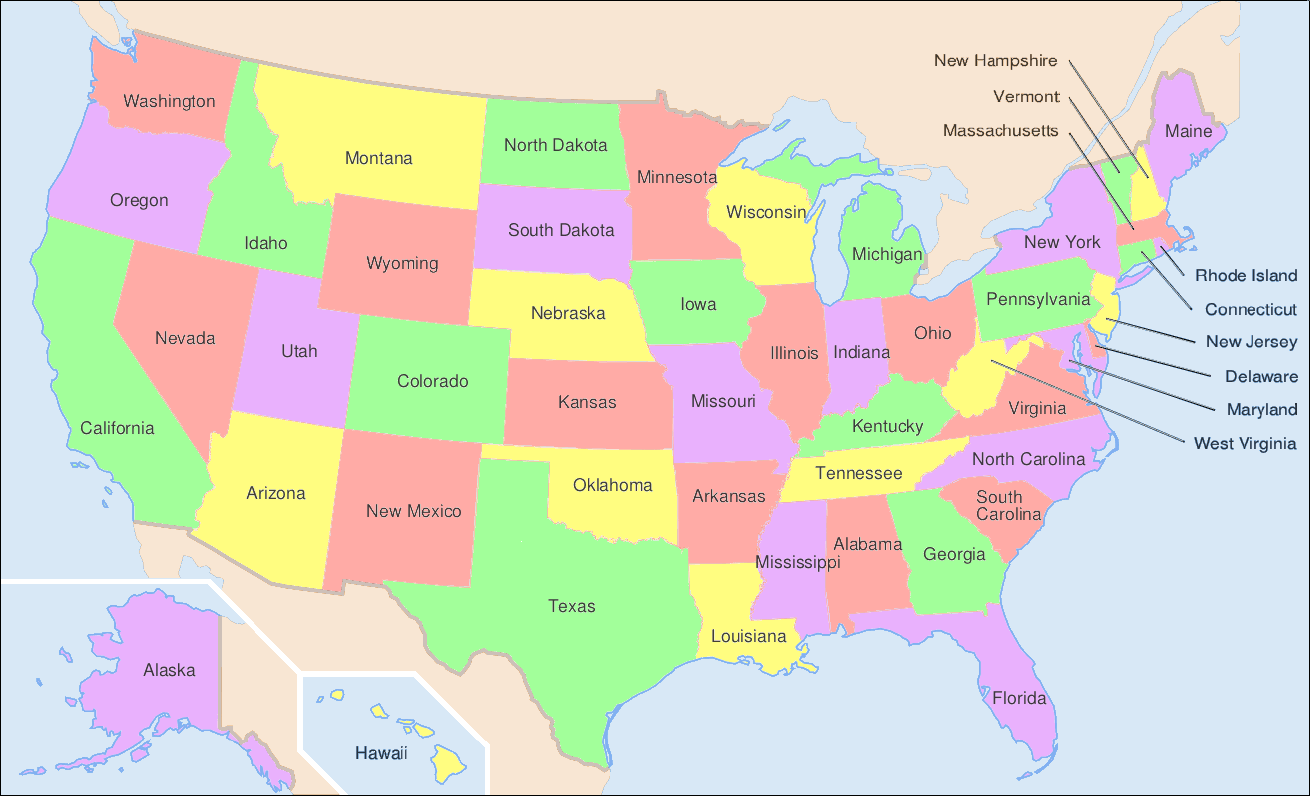
- Lyme disease has been reported in all 50 states.
- Lyme disease has been found on every continent except Antarctica.
- Ticks carrying Lyme can be smaller than the period at the end of this sentence.
- Many, perhaps most, do not get the bull’s eye rash. Some develop flu-like symptoms a week or so after becoming infected, however, many people are asymptomatic but can develop Lyme symptoms months, years or decades later.
- It is called the great imitator; looking like many other health problems (Fibromyalgia, Arthritis, Chronic Fatigue Syndrome, Bells Palsy, ADD, MS, and Lupus).
- People with other chronic disease are much more susceptible to Lyme disease, making Lyme even more likely to go undetectedcted.
- The medical community is divided over the diagnosis and treatment guidelines.
- Health insurance still often won’t cover the treatment for Chronic Lyme disease.
- Lyme Disease transmission may be possible through intercourse, and can likely be passed down through the womb.
- There are 12 strains of Borrelia that are known to cause Lyme Disease, and standard testing only tests for one.
- Lyme Disease is more epidemic than Aids, West Nile and Avian Flu combined.
- Lyme Disease can cause more than 300 different symptoms.
- The average Lyme patient takes 2-3 years to get diagnosed correctly.
- 25% of the reported cases are children.
Lyme Disease Cofactors
Leaky Gut and Lyme
In response to pathogenic toxins leaking from the intestines, the immune system produces multiple inflammatory compounds: Transforming growth factor beta-1 (TGF Beta-1), Matrix metallopeptidase 9 (MMP-9), Interleukin-1 beta (IL-1β), and Plasminogen activator inhibitor-1 (PAI-1). These inflammatory compounds affect multiple systems of the body. Because of the inflammatory compounds that become elevated in people with Lyme disease or co-infections, they are at greater risk of leaky gut. In a study on Lyme disease patients, Tumor necrosis factor alpha (TNFα) and Interleukin-13 (IL-13) were found to be elevated in different phases of infection. TNFα has also been found to be elevated in Bartonella infections, mice infected with Babesia, mice receiving Rocky Mountain Spotted Fever antigens, Ehrlichia infections, and in Brucellosis patients. Both TNFα and IL-13 have a direct effect on increasing intestinal lining leakage. Unfortunately, western medicine lacks a way to accurately diagnose and to treat leaky gut syndrome.” – Plugging the Holes in Lyme Disease Leaky Gut
I am of the opinion that a leaky gut is the root of most chronic disease. True or not, a leaky gut always exacerbates every ailment, every disease, every single health issue. You cannot cure any chronic disease without a healthy gut.
Lyme Disease and Co-infections
Ticks can carry many bacteria, viruses, fungi, and protozoans within them, and transmit these pathogens with a single bite.
The most common tick-borne diseases in the United States include Lyme disease, babesiosis, anaplasmosis, ehrlichiosis, relapsing fever, tularemia, Rocky Mountain spotted fever (RMSF). Diseases acquired together like this are called co-infections. Click below to learn more about specific Lyme disease co-infections. – About Lyme Disease Co-Infections
We also borrowed their chart:
Lyme and Candida Overgrowth
Yeast overgrowth is a common concern for Lyme patients who undergo antibiotic therapy. Whether or not the Lyme or other bacterial pathogens are killed, the immune system is depleted, the body;’s beneficial bacteria is eradicated, and the body is almost guaranteed to be overrun with fungal pathogens. If one is cured of Lyme disease they will then have to rebuild their immune system (along with healthy gut flora). Most people don’t know how to do this. If they did, they most likely would not have been susceptible to Lyme in the first place. But for those who do the Lyme treatment without successful elimination of Lyme now have to deal with a body that soon inundated with fungi.
Lyme Disease and Amalgam Fillings, Vaccines, and Other Toxic Compounds
Mercury toxicity has been linked to chronic fatigue syndrome, depression, panic attacks, insomnia, cognitive decline (Parkinson’s and Alzheimer’s, and more), chronic headaches including migraines, joint pain, Candida overgrowth, and much more. The body cannot fend off Lyme under such conditions. People with a history or poor diet, antibiotic use, mercury fillings, or immunizations, are extremely susceptible to Lyme disease and the many co-infections the come with it.
This is an excerpt from the extensive article Best Supplements To Kill Lyme and Everything Else You Ever Wanted To Know About Lyme Disease.